An email came in from a true rescuer who got involved with a man who was in cardiac arrest over the holiday while they were enjoying themselves. They cared enough to get involved and try and save this person’s life but the man stayed dead despite their attempts. This rescuer is struggling with feelings of guilt and that she didn’t do enough. In this episode, I have a very real and honest discussion with understanding living, dying and rescue.
Category Archives: CPR for Providers
Response to Post About ARVD and The Contraindications of CPR?
I received a feedback post that I wanted to respond to by video:
The post read as follows:
Roy,
My wife has a heart condition called ARVD. This involves the RIGHT VENTRICAL and the things you are asserting(about CPR) will injure or kill the person. Please see the website at Johns Hopkins on ARVD. This is a congenital heart disease that WILL NOT RESPOND TO STANDARD RESCUE PROTOCOLS. Because it involves the right ventricle the symptoms and treatments are all different. Lynn wears a Medic Alert bracelet and part of the information is to NOT perform standard CPR protocols, but to contact her doctors for information on how to proceed. She has a pacemaker and ICD, and cannot be given lidocaine or any of the standard cardiac resusitation drugs that ACLS requires. We will add that oxygen, lying on the left side and transporting to a facility familiar with heart electrophysiology, and ARVD treatment. This disease is found in athletes (runners, football and basketball players,
tennis and extreme sports) who seem on the outside to be fit, but have a heart that is not functioning as it should. This disease runs in families and it traceable through genetic testing at Johns Hopkins.
-A
It must be difficult having a loved one struggle with a cardiovascular disease as mysterious as arrhythmogenic right ventricular dysplasia(ARVD), but I want to reiterate that CPR performed by bystanders will still give more benefit than doing nothing at all.
The fact that the right ventrical is dysplastic should not have anything to do with CPR performed as an emergency intervention in order to try and circulate any increased amount of oxygenated blood to the brain and vital organs. As with everyone who goes into sudden cardiac arrest, there is no study showing that any amount of CPR would make a cardiac arrest victims biological condition worse. If left alone, and no automatic circulation and oxygenation is present, the body would continue to go without gas exchange circulation. This is why most emergency protocols, and 911 systems will encourage CPR regardless of the underlying pathology related to the cause of death. Out in the field, the goal is to keep the victim biologically alive enough to make it to the hospital or advanced care where when applicable, reversible conditions can be made right. I did contact John Hopkins and after a short discussion with an ER nurse, it was confirmed that ARVD has different protocols for cardiac arrest. Most victims of ARVD do not know they have it and therefore would present as a spontaneous sudden cardiac arrest event. If this occurs, most EMS 911 dispatch systems are going to encourage CPR. I hope this helps and I’ll let you know what I find out from the American Heart Association when they respond to my question for clarity regarding this special case. I hope this helps.
Best Wishes,
Roy, RoyOnRescue.com
Does This Cut Need Stitches? No. Well…Maybe?
In this episode we talk about the subject regarding when a cut may need to have stitches or when it can be simply treated at home. So if this question has perplexed you in the past, you may not want to miss this episode where Roy sheds some light on this sometimes confusing situation.
Happy Memorial Day Weekend!
Roy
Riding and Push Lawnmower Safety!
Have you ever been surprised by how fast a child can be in one place and the next time you turn around they are in another? Have you ever been shocked by how fast an accident can happen? In this episode, I address lawn mower safety as a result of a terrible tragedy where a 5 year old girl was hit and then run over by a riding lawn mower. It is unknown as to the exact details leading up to this horrific accident or what the abnormal conditions may have been that caused this to happen. The little girl was pronounced dead on scene. There was nothing related to first aid that would have helped her but I have to think that being more sensitive to prevention may be able to save future lives. I pray for a miraculous Grace and healing to be given to the surviving family members of this little girl and I hope to remind us all of some ways to ensure this doesn’t happen.
May God bless and heal this family.
Roy, RoyOnRescue.com
RoyOnRescue.com
My Baby Is Having A Seizure, What Do I Do?
Hello Everyone!
I received a question regarding infants having seizures and the proper treatment for them. 
The person asked if it’s proper to handle the patient the same as an adult? This is a great question and one I wanted to address a little more in depth than a simple reply by email.
First, it’s important to understand what a seizure is. The following is a quote by physician, Dr. Fawn Leigh from Duke Health who did a great job describing the two different categories of seizures and how they manifest themselves.
Click here to see the complete article located at: http://www.dukehealth.org/health_library/advice_from_doctors/your_childs_health/childhoodseizures
“Seizures are divided into two major categories (based on 1981 international classification):
- Generalized seizures affect the whole brain or both hemispheres of the brain
- Partial seizures, also known as focal seizures, affect one part or one side of the brain
Generalized Seizures
Generalized seizures are divided into convulsive and nonconvulsive. Convulsive means that there is muscle movement such as stiffening (also known as tonic) or jerking (clonic) activity. When these movements are combined it may be called “grand mal.”
Other types of convulsive seizure activity include myoclonic and atonic seizure activity. Myoclonus is usually characterized by sudden, single jerks. Atonic seizure activity is typically characterized by dropping quickly to the floor as if suddenly asleep or paralyzed. The child then quickly recovers.
These two latter convulsive seizure types can both be difficult to diagnose and treat because often they are the manifestation of a mixed seizure disorder. In infants these seizures may be called infantile spasms.
Nonconvulsive means that there is alteration of consciousness without muscle movement. This form of seizure activity was formerly called “petit mal,” and is now commonly referred to as “absence.”
Absence seizures are unique in that typically they are characterized by an abrupt onset of staring and end just as abruptly with no confused state following the events. Parents usually report that the child looks like they are “spacing out.” (Teenagers who look like this often are not having seizures — they are simply bored.)
Partial Seizures
Partial seizures can be simple or complex. Simple partial seizures are focal seizures that involve movement or sensation on one side of the body without altered consciousness. Simple partial seizures are commonly localized to areas in the brain called the motor or sensory strip.
Partial seizures may be with or without aura, which involves associated states such as fear, or changes in heart rate, flushing, or abdominal discomfort.
Complex partial seizures commonly originate from the frontal and temporal lobes of the brain where there are many complex interconnections, resulting in alteration of conscious. Typical complex partial seizures manifest as sudden change in level of alertness with or without aura, blank stare, confusional state, or aimless movements such as wandering around or repetitive behavior.”
Second, it’s important to understand what the main cuases of seizures are:
- Fever
- Infection such as meningitis
- Trauma
- Hemorrhage
- Brain malformations
- Brain dysmaturity
- Genetic disorder
Thirdly, when it comes to treating an infant compared to an adult, it’s a bit easier, though not any less intense especially if it’s your child. It’s physically easier because baby is smaller and easier to manage.
If this seizure is with a child who has never had a seizure before, 911 or Emergency Medical Services should be activated. The rescuer is going to follow National and International guidelines for treating a seizure patient. Protect the baby from hurting itself while seizing. If it’s in a bath tub, drain the bath tub of water so as to reduce the risk of drowning and then protect the child from hurting itself while seizing. Nothing should be put into it’s mouth which is old school for seizure management in trying to prevent “swallowing the tongue” or biting the tongue off. It is also important that we not try and prevent the baby’s body from convulsing by holding it still or wrapping them tightly. Simply protect it’s head and other parts of it’s body from hitting anything during the convulsive stage of the seizure. After the seizure is over, the baby will usually go into a post seizure phase called the “postictal” phase, and there may be some frothy sputum(spit) around the baby’s mouth or in its nose. A bulb syringe normally used for suctioning mucous or sinus congestion could be used to suction or clear the baby’s nasal passage but it is probably not as necessary as we’d like to think. As a general rule, baby’s have a great gag reflex and if they have any mucous or sputum in their upper airway, it will probably be coughed clear. If the baby begins to breath after the seizure, it could be irregular with some grunting for a short time and then increasingly get more normal. Skin color if it has changed during the seizure to a dusky, purple or blue color should improve as the baby begins breathing more normal and it is perfectly acceptable to comfort the baby in a natural position while maintaining a neutral airway in order for it to recover from the seizure.
If it does not begin breathing, begin basic cardiac life support according to the latest ECC/ILCOR and American Heart Association guidelines. Courtesy of ProFirstAid.com, a Free Online infant CPR training video is available by clicking here!
As many as 2-5% of all children will experience at least one seizure related to a fever over 102 degrees Fahrenheit. The seizure itself is usually harmless and does not cause brain damage nor lead to epilepsy.
Seizures in any age patient can be very scary, and the causes of a seizure are many. Therefore, if it’s the first seizure the person has ever had, we should plan for the worst and hope for the best. This can be done by calling the emergency medical services or 911 depending on your area. Support the patient with basic first aid procedures while waiting for rescuers to arrive and then follow up with your pediatrician after the baby is stable.
If your baby is having a high fever and your afraid that it may cause a febrile seizure, there are some basic steps to help lower your baby’s temperature. Click here to read an article about how to lower a body temperature from a fever.
Well, I hope this helps and I appreciate the great questions so many of you have been asking. Keep them coming and while your waiting for a response, keep on saving lives!
Best Wishes,
Roy
RoyOnRescue.com
royonrescue@gmail.com
Vomiting, Diarrhea And Dehydration, Oh My!
Some time ago, I received an emailed question asking if I could do an episode on Food Poisoning. 3 days ago, my little girl, 7, came down with symptoms that were really similar to that of Food Poisoning. After doing my own research and then calling the doctor, I thought it would be a great time to address this somewhat common and sometimes dangerous problem. Some of the suggestions given, are those that the Pediatrician gave me after my daughter had been unable to keep even a sip of water down for over 36 hours! She was pale, dry and if I’m not mistaken, it seemed like her eye sockets were indeed a bit sunken. She’s feeling better now going into hour 49 and is now holding down water, Gatorade, and a BRATY( Bread, Rice, AppleSauce, Toast, Yogurt)diet. I hope this helps anyone else who has been suffering with the flu or food poisoning. Remember, the leading reason people die from vomiting and diarrhea is due to dehydration, electrolyte imbalance and organ failure. Don’t wait until the last minute to get advanced medical attention and if it seems like the person is becoming dehydrated, get help right away. Oh, and if you’re weak or dizzy, don’t try to drive yourself in to the hospital…that’s what 911 is for!
Best Wishes and God bless you as we enter into this most Holy season of Easter,
Roy Shaw, RoyOnRescue.com
Get This Car Off My Chest!
In this episode of RoyOnRescue, Roy received a question from an EMT student who was trying to learn more about traumatic asphyxiation. The EMT student wanted more information about this traumatic injury. Many times these injuries happen as a result of a very heavy object dropping onto a persons chest and trapping the person under it’s weight. It’s important to recognize the emergency and take action right away. You won’t want to miss this episode of RoyOnRescue.
Professional Rescuers and Good Samaritan Act Part 2
I had a royonrescue.com reader who had a concern that the post about the Good Samaritan Act might scare rescuers into not providing care while off duty. I think this may have been a misunderstanding and I must clarify that I’m speaking to medical professionals that have training and expertise in the area of rescue, not those volunteers, family members, bystanders without any training who may want to try and get involved. Below is the comment from this individual and my response back to them with references. I hope this helps anyone else who may have had the same concern or question.
Question/Comment: 4-3-11
Dear Mr. Shaw,
I found your video, Professional Rescuers and The Good Samaritan Law, discouraging. I agree with just about everything you advised, but I have one major complaint. You said, “You can do care up to a specific level. In fact, that of which you are trained to do proficiently.” I think what you have said is misleading.
If you apply those restrictions to Good Samaritan laws, you defeat the intent of those laws*. Here’s a quick example: I would guess that 90% of civilians who have taken CRP classes (as I have) are not proficient in CPR. They have a good idea what CPR is, but in an emergency with the adrenalin flowing, I can see them making numerous missteps, which may or may not affect the outcome. According to your advice even a Red Cross card carrying volunteer should not attempt CPR because he/she is not proficient. And what about the AEDs appearing in malls and schools? According to your advice, the average passer-by who’s had no training should only call 9-1-1 and leave this new fangled equipment for the experts! I’m sure that is not what you would advise.
Then, there is the example of your buddy, the snowmobiler, with the crushed & torn larynx. It sounds like you let him die? You knew what needed to be done, a surgical tracheotomy. Of course your snowy scene was “an uncontrolled environment”. Isn’t that’s why it’s an “emergency”. You had the equipment and you had the training, but you chose not to do that which you could do. Personally, I think you should have at tried. (Jas 4:17) Sure, like you said, the scene was far from perfect but you had what you needed to perform the procedure. And yes, you may be right, there’s a good chance you would not have been successful. But if your friend could have, don’t you think he or his wife would have wanted you to at least try?
Instead of encouraging guys like me to do what they reasonable can, you’ve lead us to believe we need to be trained or we will be held liable for trying. The best way to ensure that one follows your advice to “Do No Further Harm” is to look the other way.
FYI: I carry Celox & QuikClot, which I know state protocols does not allow EMTs and medical professionals use. I’ve never used it nor been trained, but if on the firing range someone gets shot and I have no other means to stop a bleed out, I intend to try it. Hopefully, I will never be put to the test on the highway or the rifle range, but despite your warning about “level of training” and “proficiency” it is an option I may have to pick.
Despite my disapproval of this video, I have check out some of your other stuff and I think you do a pretty good job, esp. your written responses (unlike mine).
Thanks for sharing
My Response:
Hello “Name Not Disclosed” ,
I appreciate you taking the time to respond to the royonrescue.com blog entry, “Professional Rescuers and The Good Samaritan Law”.
I wanted to clarify the “providing care up to ones level of trained proficiency”.
The Good Samaritan Act in the State of Michigan states;
“691.1501 Physicians, physician’s assistant, or nurses rendering emergency care or determining fitness to engage in competitive sports; liability for acts or omissions; definitions.
(1) A physician, physician’s assistant, registered professional nurse, or licensed practical nurse who in good faith renders emergency care without compensation at the scene of an emergency, if a physician-patient relationship, physician’s assistant-patient relationship, registered professional nurse-patient relationship, or licensed practical nurse-patient relationship did not exist before the emergency, is not liable for civil damages as a result of acts or omissions by the physician, physician’s assistant, registered professional nurse, or licensed practical nurse in rendering the emergency care, except acts or omissions amounting to gross negligence or willful and wanton misconduct.
(2) A physician or physician’s assistant who in good faith performs a physical examination without compensation upon an individual to determine the individual’s fitness to engage in competitive sports and who has obtained a form described in this subsection signed by the individual or, if the individual is a minor, by the parent or guardian of the minor, is not liable for civil damages as a result of acts or omissions by the physician or physician’s assistant in performing the physical examination, except acts or omissions amounting to gross negligence or willful and wanton misconduct or which are outside the scope of the license held by the physician or physician’s assistant. The form required by this subsection shall contain a statement indicating that the person signing the form knows that the physician or physician’s assistant is not necessarily performing a complete physical examination and is not liable under this section for civil damages as a result of acts or omissions by the physician or physician’s assistant in performing the physical examination, except acts or omissions amounting to gross negligence or willful and wanton misconduct or which are outside the scope of the license held by the physician or physician’s assistant.
(3) A physician, physician’s assistant, registered professional nurse, or licensed practical nurse who in good faith renders emergency care without compensation to an individual requiring emergency care as a result of having engaged in competitive sports is not liable for civil damages as a result of acts or omissions by the physician, physician’s assistant, registered professional nurse, or licensed practical nurse in rendering the emergency care, except acts or omissions amounting to gross negligence or willful and wanton misconduct and except acts or omissions that are outside the scope of the license held by the physician, physician’s assistant, registered professional nurse, or licensed practical nurse. This subsection applies to the rendering of emergency care to a minor even if the physician, physician’s assistant, registered professional nurse, or licensed practical nurse does not obtain the consent of the parent or guardian of the minor before the emergency care is rendered”. http://nspc203.com/leg/MichiganGoodSamaritanActForMedicalProfessionals.htm
And in one other source I found an explanation that goes on to describe the Good Samaritan Act this way; “While Good Samaritan laws vary from state to state, these laws typically apply when you take purely voluntary, good-faith action to help another person at the scene of an emergency, and the person does not object to your help. If you provide help to another person under a Good Samaritan law, keep in mind that you must exercise the same standard of care and/or treatment that you normally help to in your profession. In other words, if you’re a trained medical professional, then you must act according to medical professional standards. However, if you are not trained in a medical professional, then your duty may be only to call for help or other forms of help, but not to render medical care or first aid. So long as you act reasonably in light of the circumstance, and in keeping with professional standards, you probably will not be liable in a jurisdiction that has enacted a Good Samaritan law”.
http://resources.lawinfo.com/en/Articles/personal-injury/Federal/what-are-good-samaritan-laws.html
So you see, this is why no matter how much I would like to re-assure professionals that they are completely safe when rendering aid and especially “creative solutions medicine” to a person without repayment as a Good Samaritan, the professional still needs to understand that because of their training, they do have a duty to perform to a “standard of care” appropriate for their profession even if it’s frustrating and they may think that they can do more.
Individuals who offer Good Samaritan aid and have never been trained in any medical area may not be held to the same standards if they are sued, but the original blog was directed toward those with training and professional expertise in the area of rescue which is a different scenario.
I hope this helps to clear up any misunderstanding or confusion and please don’t hesitate to contact me for more clarification or for any future subjects down the road.
Best Wishes,
Roy Shaw, RoyOnRescue.com
royonrescue@gmail.com
Allergic Reaction and No Epi Pen!
I received another email from a person asking: “What are basic first aid measures for a serious allergic reaction if there is no epi pen available? I watched your training video in your library at ProFirstAid.com but I can’t seem to find an answer.”
Thanks for your answer,
C
Thanks for the question C. I thought this was a good question and a situation which no one wants to find themselves. So I decided to reply back and include it into the RoyOnRescue.com blog response. I hope it helps.
Here’s my reply:
Dear C,
Other than immediately calling EMS/911, if at all possible, let the person rest in position of comfort.
Some of the things that are indicated for first aid providers are:
1. Watch for signs and symptoms of severe allergic reactions like difficulty breathing, itching, hives, swelling, sore throat, anxiety.
2. Remove victim from anything that would aggravate or worsen the symptoms.
3. Give supportive care like rescue breathing, CPR, shock treatment etc when indicated.
4. If at all possible, identify what it is that gave the person their serious allergic reaction and avoid any further exposure to it.
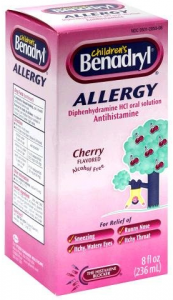
This is not a prescription but simply something that I would do. I always like to have liquid diphenhydramine(Benadryl like antihistimine) on hand that can be taken as prescribed on the container or per doctors order. If I did not have a prescription for a “rescue inhaler” like albuterol or didn’t have an allergy response kit prescribed and filled from my doctor I would really emphasize doing so, and then keeping it up to date as the epi pen and other medications could expire and be useless.
Remember, recognizing the early signs of an allergic reaction and activating EMS/911 as soon as possible is critical. Time is of the essence. Oh! And if you think you may have an allergy, or have ever had a severe allergic reaction, you should be sure to contact your medical professional and get a filled prescription for an emergency allergic reaction kit, AKA: bee sting kit.
I hope this helps, and best wishes.
Roy
Follow Up Comment to Chest Injuries and CPR
I received a question from a person who after watching the “Chest Injuries and CPR” video blog asked:
Dear Roy,
Reading your letter, I would agree if the injury is just soft tissue injury. However if a # is suspected, It would be dangerous to do CPR as the # might or will puncture the lungs and cause immediate death, if immediate intervention is not available.
Kindly comment.
Here is my response:
Hello,
Regarding your question about Chest Injuries and CPR. It’s important to make a distinguishing point whenever we talk about CPR. When a person is in need of CPR, it means that the person is in cardiac arrest. This is to say that they are unconscious, not moving, not breathing normally. If this is the case, they are presumably in cardiac arrest or in a state that justifies Cardio Pulmonary Resuscitation.
If the person needs CPR, this means that they are clinically dead. If the victim does not receive CPR, they will simply graduate to permanent death otherwise known as biological death(permanent).
This is why, regardless of the chest injury, if the person is “dead” or in need of CPR, compressions are to be given per the American Heart Association guidelines even if the complications could include those of punctured lungs, lacerated organs, or bruised/punctured heart muscle. This would be based on the theory that a person in need of CPR is already dead and will not be harmed more even if there are negative side effects from providing chest compressions. If a person remains dead, surgery is not an option but if the person is resuscitated with CPR, and alive at the hospital, we have an opportunity to fix the injuries that may have been aggravated by doing CPR.
If however, the person is awake, is breathing normally and therefore does not appear to need CPR, it would be correct that chest compressions and CPR may complicate the already damaged chest and complicate the victims injuries. As soon as the victim becomes unconscious, is not breathing normally and now appears to need CPR, Emergency Services would be contacted and CPR would be initiated regardless of the injuries of the patient.
I appreciate the question and hope that this clarifies any confusion caused by the article. Please don’t hesitate to email me again if you would like to continue dialogue on this subject.
Best Wishes,
Roy Shaw, RoyOnRescue.com
royonrescue@gmail.com