In this episode of RoyOnRescue, I answer a question from someone who jumped feet first into a shallow pool and now their foot hurts when they walk on it. Is it broken or just sprained and how do I know what to do? Watch this episode to find out more.
Category Archives: Training Questions
I Have Throat Ulcers! Now What!?
I received an email from a Rescue Fan that had a severe soar throat and wasn’t sure if she should go to the doctor. I suggested they do, and she was diagnosed with throat ulcers. I thought I’d do a RoyOnRescue to help explain what they are and why you should see a doctor. I hope it helps.
How Do I Survive A Heart Attack Alone?
It can be very scary to have a medical emergency but even more scary if you’re all alone with no one to help. In this video, I explain what to do if you have chest pain or you think you’re having a heart attack and your alone.
If you’ve ever wondered what to do when you’re experiencing a medical or life threatening emergency and you find yourself alone, you may get the answer you’re looking for right here, on this episode of RoyOnRescue!

How Do I Treat Neck Injuries On The Ice?
In this episode we answer a question that was sent in by a Rescue Fan that wondered what the best course of action would be if a person suffered a neck injury on the ice. It’s important to remember that if the patient has any pain, movement minimization is the goal while maintaining the patients core body temperature while waiting for EMS to arrive. If the person doesn’t feel hurt, they may elect to slowly get to their feet and recover. If they do feel pain, numbness, tingling, weakness or loss of consciousness, the best course of treatment  in my opinion is to call 911 or EMS. I hope it helps.
in my opinion is to call 911 or EMS. I hope it helps.
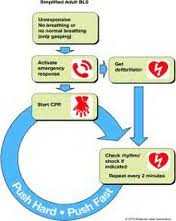
Why the phrase “Not Breathing Normally?”
I saw a comment come in this morning from our training feedback report that read, “in your trainings, why do you say, ‘not breathing normally’ instead of ‘not breathing,’ period, for starting CPR?” I thought this was a valid question and so I thought I’d try to reply with a valid answer! The following is my reply to their question. I hope it helps.
Email Questions and Answers Part 1
Hello Everyone!
In this episode of RoyOnRescue, Roy takes some time to catch up on different emailed questions and comments that have come in over the last few months. The two different emailed questions that were answered were; “won’t laying a person down while choking only make it worse?” and “I thought we were always suppose to control arterial bleeding before beginning cpr!”. Roy takes his time to discuss these two different topics and explain the reasons why we do what we do in rescue in detail.
Be sure to join Roy in Part 1 of several parts as he works his way through a list of different topics that have been sent in by viewers like you.
Remember, If you’ve got a question or comment that you would like Roy to answer or give a response, please send it via email to: royonrescue@gmail.com. Be sure to follow Roy on twitter at: @royonrescue
Remember, your actions make a bigger difference than you realize and you can change the course of history.
Keep On Rescuing,
The RoyOnRescue Team
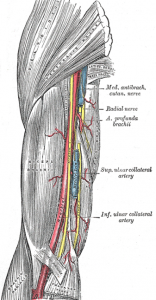
Follow Up Answer Based On Question Regarding “How To Find The Brachial Pulse”
Hello Everyone,
Great follow up question came in on how to locate the “brachial” artery.
It’s located on the inside of the upper arm between the biceps and triceps muscle along the humerus bone. Use the flat part of your four fingers to press moderately against the inside of the arm at this location. This is a skill that needs practice with a baby who has pulses so as to be confident when looking for a brachial pulse on a child without a pulse. Remember, when in doubt, if the patient is unconscious, not breathing normally and appears dead…we treat them as they are. Begin CPR!
Hope it helps.
Roy
“Why Are There Different Names For Different Pulses?”
Today I had a great question come in through our customer solutions department. Here’s what it said.
“What and why are the pulses of different ages called different things and what are they called?”
Well, I understood this to mean, what are the different locations for the different age groups in cardiac arrest or unconsciousness and so I gave the following answer.
Hello,
Thank you so much for your question. It’s a great question and I think I might be able to shed some light on it.
It can be a little confusing some times as we try and decode the reason why certain things in medicine are named what they are. Basic Life Support is not immune to this same situation. In regards to the names of “pulses” and how they are named according to the age or size of the patient, I’ll try to clarify.
If I understand your question correctly, you’re talking about the three locations of the pulse check.
1. Radial, which is found in the wrist of the patient, usually used for patients who are adult or child size. Older than 1 year of age. This location is used for general pulse rate and quality but not usually for the unconscious patient.
2. Brachial, which is found in the bicep/tricep region of the upper arm on the inside of the arm. This is the location for an unconscious infant, age 1 year or younger.
3. Carotid, which is found in the neck. This would be located between the trachea and the sternocleidomastoid muscle(located on the side of the neck). One can really see this muscle well when one turns their head to one side or the other. This would be the location of choice for the adult and child(older than 1 year) unconscious patient.
There is yet another location used in emergency medicine but not usually pre-hospital and that would be the femoral artery. This is located in the groin of the patient and again is usually used for trauma patients that have C-Spine collar or the carotid is not easily accessed due to intubation etc.
The reason to use the brachial over the carotid for an infant is primarily due to the fact that most baby’s don’t have necks to speak of. They have milk catching folds of skin but other than that, their anatomy is such that an area to evaluate an accurate carotid pulse is not easily obtained. Therefore, the brachial artery is the location of choice and works extremely well for the health care professional to ascertain whether a pulse is present or absent.
In most cases for adults and children over the age of 1 year, the carotid artery is the location of choice to check for pulse presence due to it being the last place to feel a pulse prior to the blood pressure being too low to feel a pulse regardless of whether the heart is beating or not. Secondly, it’s next to the location where we are performing a head tilt and chin lift while giving rescue breaths and is convenient to the rescuer for checking pulse presence(little perk).
So, though the names of the locations can be a little challenging, they do make great scrabble words, or can make you look really intelligent at dinner parties. Remember, it’s not the feeling of a pulse that will determine if we’re going to start cardiac compressions or not, It’s the absence of signs of life that will determine that. This includes, unconscious and unresponsiveness and that the patient is not breathing normally or not breathing at all. If these two signs are present, begin CPR. Pulse checks have often given false readings and postponed cardiac compressions in a patient who needed cardiac compressions desperately.
I hope this helps anyone who may have had the same question.
Best wishes and keep on rescuing!
Roy
RoyOnRescue.com
—
Roy W. Shaw, EMT-Paramedic
Director of Training and Compliance
ProTrainings.com
Can Anyone Use An AED?
In this mobile vlog, Roy wanted to address the AED question asked by two different people at almost the same time. Though there may be slightly different legal rules in the U.K. Compared to the U.S., both countries follow closely related ILCOR recommendations/guidelines. Always check your local laws to be sure, but in this episode, Roy addresses what the 2010 guidelines changed and why you can probably use an AED without any formal training. Let him know what you think of his more mobile format. He’s trying a new app that would allow him to record and post from almost anywhere and anytime. Not as finished as the in-studio videos but let’s him be more efficient. He will use the other format too but will sneak in some simpler ones when time is crunched. Your comments will be appreciated. Send comments to: royonrescue@gmail.com.
The RoyOnRescue Team

Here’s A Test Question. You’re At The Scene Of A Car Accident…
In this episode of RoyOnRescue, Roy replies to a comment that was submitted by a student who questioned the logic as to why ProTrainings.com offers a test that would give a scenario about a car accident when it wasn’t specifically covered in the training. Roy helps shed some light on this by applying the basic principals of basic CPR and First Aid as it relates to “Scene Size Up”, Scene Safety, and patient assessment. He also shows how the universality of Emergency First Response can usually be applied to almost every situation.