In some cases it has! The velocity of an object striking one’s chest can cause a phenomenon that could disrupt the normal beating heart. If this happens, everyone standing by should hope they can recognize it, and treat it. Here’s how I got on this subject.
An email came in to our offices asking about more information regarding what happens when a child is struck in the chest or abdomen ,ith a ball, puck, bat or other hard object.
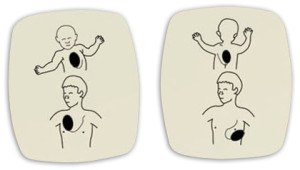
Sports can be fun but not when someone gets seriously hurt or dies. One type of injury that is a real concern to everyone is cardiac arrest secondary to chest trauma from a blunt object. This can happen when a baseball, soccer ball, basketball, hockey puck, bat or person hits another persons chest with a great deal of velocity or force.(http://pediatrics.aappublications.org/cgi/content/full/122/2/437) In some cases, it is suspected that if a ball or other object hits a person chest over the top of the location of the heart, the strike works somewhat like a technique that was once used to mechanically cardiovert a heart called a precordial thump(http://www.heartrhythmjournal.com/article/S1547-5271%2809%2900687-0/abstract). This technique used force vs. electricity to create some form of rhythm or Arrhythmia/ Ventricular Fibrillation in order for the heart to be corrected so as to regain a purposeful and organized heart rhythm. This technique though used rarely today, may be the effect that is causing sudden cardiac arrest in children and adults who are involved in a chest trauma from sports. If this does happen, the person may collapse immediately and stop breathing with no palpable(you can’t feel it) pulse. If the person is in cardiac arrest or is not showing signs of life, 911/Activation of EMS and CPR should be started immediately and an AED may be very useful if the person is in a shockable condition. If an AED is not present, CPR will be done continuously without interruption unless the person becomes conscious and begins to move or attempts to speak(signs of life). Be on guard, bruising, punctured lung or other underlying conditions could cause the person to return to a state of cardiac arrest so frequent reassessments will be required until the person is turned fully over to the care of emergency medical services. The best cure for this injury is prevention. Many companies are designing and selling chest guards and protective devices to help prevent this condition from happening.(http://www.allsportsarmour.com/CHEST_ARMOUR_SHIRT_p/asa100%20dual.htm A well trained professional or volunteer coaching team in CPR and First Aid (http://www.profirstaid.com)would be highly suggested and an AED can be purchased for less than a laptop today.(ProFirstAid.com)
In comparison another condition related to a blunt trauma to the abdomen is a condition nick named, “getting the wind knocked out”. This condition usually occurs when a person receives a blow to the upper center abdomen which is approximately where we provide inward and upward abdominal thrusts for a choking victim. This area is physiologically perfect for compressing the diaphragm and compressing the lower lobes of the lungs. This forces residual air out of the lungs and feels scary. Normally, after a few minutes of one trying to breath deeply, fighting hard for that first real deep breath, the spasm releases in the diaphragm and air is gradually brought back into a normal state. Complications related to this fairly common condition could include ruptured or torn internal organs. If a person is hit hard enough, as in situations where a bat or object was used, or the lower half of a steering wheel which is common in unrestrained, non airbag vehicular accidents, the trauma could rupture/tear internal organs and even the descending aorta. If the Aorta is torn or ruptured, it is well know to be a usually fatal injury as time to surgery is quite a few minutes away and one can loose enough blood internally to die from hypovolemia. A condition where there is not enough blood to circulate oxygenated blood or maintain an adequate blood pressure which leads to death if not corrected. Treatment for this more serious condition is activation of emergency medical services while providing CPR, Shock Therapy(http://www.profirstaid.com) and minimization of movement. A way to prevent this injury is to avoid the types of conditions that could present it. Another way is to incorporate an aggressive core strength training program which will build strength in the abdominal muscles so as to help protect against sport related injuries.
It is important to consult with your health care professional or physician before beginning any intense workout program and if you are at all concerned that you or someone you know may have internal injuries, call 911/EMS and seek medical help.
Most of the signs and symptoms related to an internal injury in the chest or abdomen are severe pain that disables a person from performing normal behaviors. Tender abdomen to touch, distending(bulging) belly, rigid or hard belly) bruising or marks over the abdomen or chest, shortness of breath or difficulty breathing, pale, cool, sweaty, increased anxiety, increased respiratory rate, dizziness, fear of dying and unconsciousness. If any of these signs or symptoms are present or appear after an injury, activate the Emergency Medical Services immediately and/or seek medical help right away.
I hope this answers the question and I hope the next time you are by someone who is struck in the chest or simply gets the wind knocked out of them, you’ll better know what it is, what to do, and how to help.
Best Wishes,
Roy Shaw, EMT-P, RoyOnRescue
www.royonrescue.com
Tweet: @royonrescue
P.S. Here’s a link to a real life scenario. It’s worth the read Mom and Dad.
http://www.huffingtonpost.com/2008/05/19/family-of-boy-hit-by-base_n_102439.html