In this RoyOnRescue Video blog, Roy takes a look at the record breaking heat that most of the Country has been experiencing and gives a few tips on recognition and treatment of heat related emergencies like; heat exhaustion, heat stroke, dehydration, electrolyte problems etc. So learn what to do, and how to survive the severe summer heat. Don’t miss this episode of RoyOnRescue!
P.S. Below, I’ve included some really clear signs and symptoms of heat related injuries, compliments of WebMD. Click on the WebMD link for more information.
What Are the Symptoms of Heat-Related Illnesses?
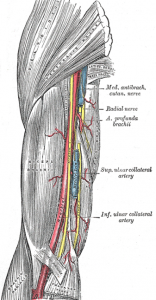
Heat cramp symptoms include:
- Severe, sometimes disabling, cramps that typically begin suddenly in the hands, calves, or feet
- Hard, tense muscles
Heat exhaustion symptoms include:
Recommended Related to First Aid
- Fatigue
- Nausea
- Headaches
- Excessive thirst
- Muscle aches and cramps
- Weakness
- Confusion or anxiety
- Drenching sweats, often accompanied by cold, clammy skin.
- Slowed or weakened heartbeat.
- Dizziness
- Fainting
- Agitation
Heat exhaustion requires immediate attention but is not usually life-threatening.
Heat stroke symptoms include:
- Nausea and vomiting
- Headache
- Dizziness or vertigo
- Fatigue
- Hot, flushed, dry skin
- Rapid heart rate
- Decreased sweating
- Shortness of breath
- Decreased urination
- Blood in urine or stool
- Increased body temperature (104 to 106 degrees)
- Confusion, delirium, or loss of consciousness
- Convulsions
Heat stroke can occur suddenly, without any symptoms of heat exhaustion. If a person is experiencing symptoms of heat exhaustion or heat stroke, GET MEDICAL CARE IMMEDIATELY. Any delay could be fatal. Seek emergency medical care for anyone who has been in the heat and who has the following symptoms:
- Confusion, anxiety, or loss of consciousness
- Very rapid or dramatically slowed heartbeat
- Rapid rise in body temperature that reaches 104 to 106 degrees Fahrenheit
- Either drenching sweats accompanied by cold, clammy skin (which may indicate heat exhaustion); or a marked decrease in sweating accompanied by hot, flushed, dry skin (which may indicate heat stroke)
- Convulsions
- Any other heat-related symptom that is not alleviated by moving to a shady or air-conditioned area and administering fluids and salts