Hello Rescuers!
I just received a question via our ProCPR customer feedback that read: 
Dear ProCPR, “Question 16 says you have on PPE (personal protective equipment) already, then you check for
responsiveness. Why would you put on your PPE before you check consciousness?
– Anthony
In case anyone else may have asked the same question I though I’d address it. First, Question 16 is the number this person was on while taking the ProCPR.org test. This is the online portion of the Health Care Provider level BLS certification training in case anyone was wondering.
Okay, now for the answer. As professional health care providers, we should always be thinking about cross contamination. We don’t want to catch what the patient may have and we don’t want to give the patient anything that we may have! Remember, PPE works both ways. Can anyone say, nosocomial infection? Even if the patient isn’t in obvious distress or obviously infectious, we should be thinking about the fact that the person seems to be in need and may require medical treatment. This means that we may need gloves, CPR shield with one way barrier, goggles, face mask, respiratory protection etc. This is why it’s so important to think about PPE whenever we encounter a situation that may call us into action. Not just when the person is unconscious or not breathing.
Forever, I’ve battled the problem with health care professionals short cutting PPE while giving care or even thinking about care. We really do need to consider the two way protective properties related to infection control as it relates to appropriate personal protective equipment.
When it comes to layperson rescue, one of the top five reasons that laypeople will not intervene when a person is in distress is the fear of disease! If the rescuer is approaching a victim and dons their gloves early as well as ensures that they have a CPR shield available, the fear of catching a disease is greatly diminished. This will increase the chances that the Good Samaritan may actually get physically involved in the rescue.
Now I know what you may be thinking…”Roy! Do you really think that I’ll have one of those rescue kits on by belt all the time? You may be a “Rescue Hero” type but the feasibility of me having PPE on my person when I’m at the beach, shopping, walking, vacationing, or even at a business meeting is slim to none.” Well, I have to agree! Unless you are a professional rescuer on duty, you probably won’t have your jump kit, glove pouch or a one way valve mask bag swinging from your belt loop. So how will you have the PPE you need at the time you need it? The best way I’ve found is to have a key ring rescue kit. The catch is having it be small enough to not get in the way and large enough to carry your gloves and a one way CPR shield. The reason I say a Key Ring style, is that I think that keys are the one item that most people have with them most of the time. If they don’t have them with them, then they are usually close at hand. And if we have our keys, we’ll at least have gloves and a CPR shield. So make sure you get one and then the PPE problem is out of the way. Still don’t think that PPE is needed? Well, that’s why the AHA endorses “hands only” CPR! It’s really not that compression only CPR is better than full Cardio PULMONARY resuscitation, it’s that there are so many non PPE toting people afraid that they may catch a disease if they do mouth to mouth rescue breaths that we had to design a new form of bystander CPR. Since implementing “Hands only” CPR, there has been an increase in rescuer involvement. And when people get involved and provide CPR, lives are saved!
PPE should be on every rescuer’s mind…and key chain, lay or professional and when we begin to think about PPE as the first step in rescue, lives are saved and infection is prevented more often!
Hope this helps.



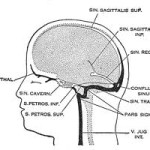 plained it but he was still a bit foggy regarding the diagnosis. Well, after looking into it from the clinical perspective, I realized that it was a pretty big deal and in some cases may be fatal. I researched multiple sources to gather credible information and when it all came down to brass tacks, I found that the Wikipedia explanation had done a pretty dog-gone good job of summarizing
plained it but he was still a bit foggy regarding the diagnosis. Well, after looking into it from the clinical perspective, I realized that it was a pretty big deal and in some cases may be fatal. I researched multiple sources to gather credible information and when it all came down to brass tacks, I found that the Wikipedia explanation had done a pretty dog-gone good job of summarizing 



